Top Tips: Glycemic Index For Diabetes Management
The importance of glycemic index (GI) has become a cornerstone in managing diabetes. Simply put, the Glycemic Index (GI) is a ranking system for carbohydrates based on their immediate effect on blood glucose levels. Carbs with a high GI spike blood sugar rapidly, while those with a low GI have a slower, more gradual impact.
For anyone managing diabetes, understanding and utilizing the GI of foods is crucial because the right choices can lead to more stable blood sugar levels over time. Typically, the food categories are low (55 or less), medium (56-69), and high (70 or higher) GI.
The relevance of GI extends beyond simple classifications. Certain fruits, for instance, might surprise you with their low GI despite being sweet. Meanwhile, some starchy foods might have a higher GI than expected. Complexity aside, using GI as a resource can help you navigate dietary choices and, in turn, better control your diabetes.
Incorporating Low GI Foods into a Diabetic Diet
Managing your blood sugar is paramount when you have diabetes, and incorporating low glycemic index (GI) foods into your diet can be a game changer. We digest and absorb low-GI foods more slowly, causing a gradual rise in blood sugar levels and reducing the risk of triggering hyperglycemia.
As a staple of a well-managed diabetic diet, low GI foods help maintain blood glucose levels within the target range. They provide a steady energy source and can prevent the typical highs and lows associated with diabetes.
Common low-GI foods include whole grains like barley and oatmeal, legumes such as lentils and chickpeas, and non-starchy vegetables like leafy greens and peppers. Fruits that feature lower on the GI scale, such as apples and berries, are also excellent choices.
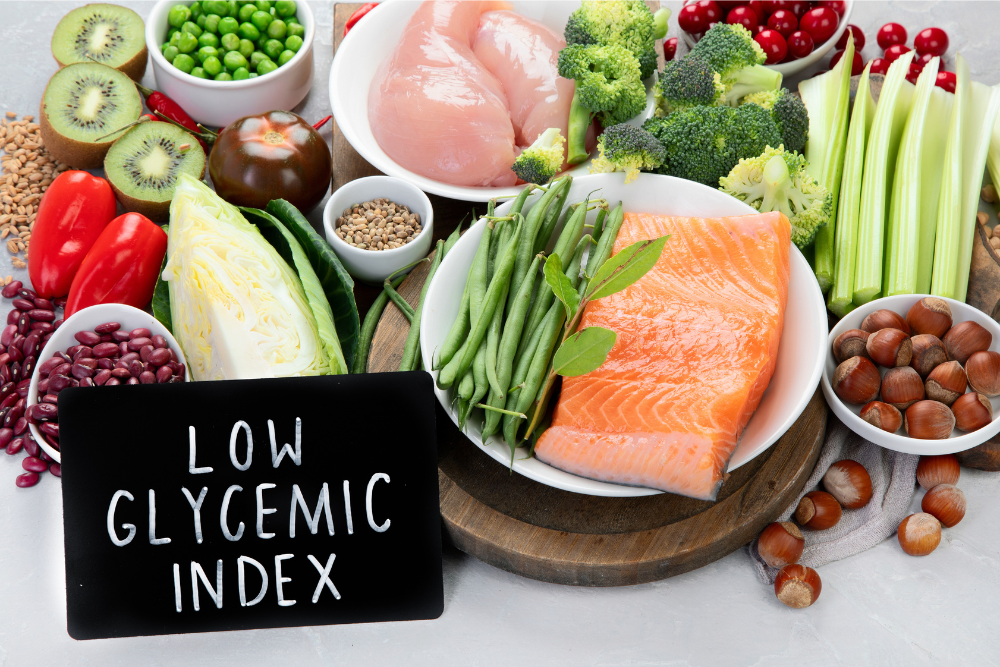
Meal planning should shift focus toward these foods. Replace white bread with whole grain varieties, choose steel-cut oats instead of instant oatmeal, and favour fresh fruits over juices. In the kitchen, aim for cooking methods that preserve the integrity of these foods — think steaming, roasting, or grilling.
Balancing Your Plate: Combining GI With Other Nutritional Considerations
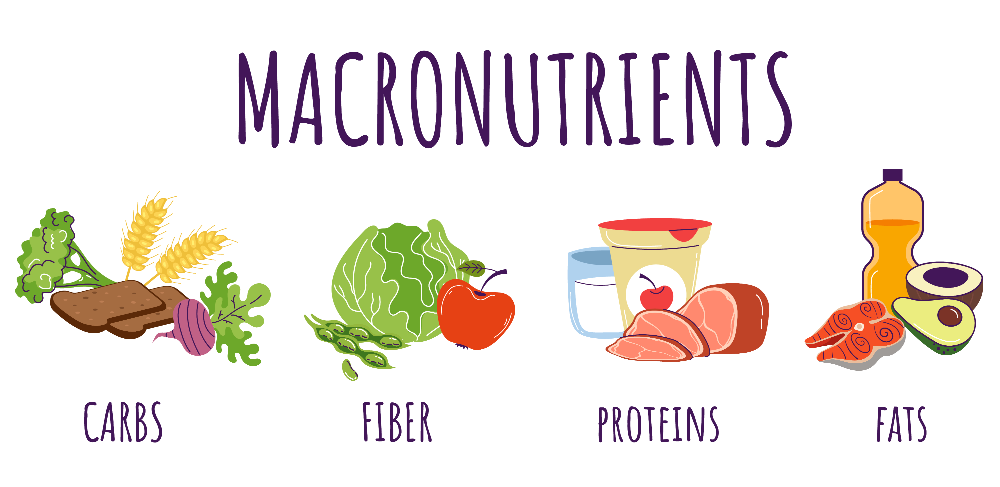
When managing diabetes, honing in on the glycemic index is crucial, but it’s not the whole picture. Nutrition is multidimensional, and it’s essential to create a balanced plate that includes a variety of nutrients, not just focusing on the GI values alone.
The glycemic index is one tool in the toolbox; consider it your guide for how quickly certain foods can affect your blood sugar levels. However, you also need to pay attention to the overall nutritional value of your meals. This balance helps ensure your body receives the essential nutrients while managing your blood glucose levels effectively.
Fibre is a key player here. It can help manage blood sugar by slowing the digestion and absorption of sugars, meaning high-fibre foods are often associated with lower Glycemic Index scores. Additionally, fibre supports digestive health and can help you feel full for longer, so foods rich in fibre, like vegetables, lentils, beans, and whole grains, are staples in a diabetes-friendly diet.
Protein is another essential macronutrient. It doesn’t directly impact blood sugar levels as carbohydrates do. Still, it’s vital for building and repairing tissues and maintaining muscle mass. Including a source of lean protein in every meal, such as fish, poultry, or tofu, can contribute to overall meal satisfaction and help prevent blood sugar spikes.
Lastly, healthy fats benefit heart health – an essential consideration since diabetes can increase heart disease risk. Foods like avocados, nuts, seeds, and olive oil provide these fats. They can also moderate the glycemic response when paired with carbohydrates.
Creating a well-rounded meal involves consciously including low-GI foods alongside sufficient fibre, lean protein, and healthy fats. This way, you can maintain a steady energy release, stay full for longer, and maintain your blood sugar levels within the desired range.
Remember that portion sizes matter, too; even foods with a low GI can cause blood sugar spikes if consumed in excess. Using the glycaemic index as a starting point, look at the big nutritional picture, and you can make smarter, more informed decisions about what’s on your plate.
Personalized Glycemic Index Management: Tailoring GI to Your Lifestyle
If you’re navigating the waters of diabetes management, you may have realized that what works for someone else might not work for you. Understanding the glycemic index is important, but it’s also essential to recognize that people with diabetes can respond differently to the same foods.
To create an efficient and personalized meal plan, you should observe how your body responds to various foods. Tracking your blood sugar levels after meals can give you a clearer picture of how specific low, medium, or high Glycemic Index foods affect your glucose readings.
Lifestyle plays a crucial role as well. For instance, your level of physical activity, the timing of your meals, and even your stress levels can all influence how your body processes carbohydrates. A dietitian can help tailor your meal plan, considering both the GI of foods and your lifestyle variables.
Medications might also impact your blood sugar responses. If you use insulin or other diabetes medicines, understanding the interplay between your diet’s Glycemic Index and medications is critical. Some foods might be more compatible with your current treatment regimen than others.
Remember, managing diabetes is a dynamic process. What and when you eat, how much you exercise, and how well you manage stress are all parts of the equation. A holistic approach that customizes your diet to fit your lifestyle is often the most realistic and sustainable route to stable blood glucose levels.
Beyond the Index: The Future of Diabetes Management and GI Research
While the glycemic index has significantly improved how individuals manage their diabetes, the journey doesn’t end there. Innovations in science and medicine continually shed new light on optimizing blood sugar control through dietary choices.

Researchers are tirelessly working to investigate how different food combinations and preparation methods might affect glycemic response. Refining our understanding of the GI and its practical application in diabetes care will enable even more personalized diet plans.
Emerging technologies, including continuous glucose monitors and intelligent insulin pumps, have started integrating with mobile apps and health platforms. These advancements may provide real-time feedback on how specific foods influence an individual’s blood sugar and offer immediate dietary adjustments.
Artificial intelligence and machine learning promise to revolutionize diabetes management. Predictive models based on large datasets could provide individuals with unparalleled insights into their unique glycemic responses, tailoring dietary advice to maximum precision.
As we look forward, embracing these developments and staying informed will be crucial. The dialogue between patients, healthcare providers, and researchers must continue to evolve, ensuring diabetes management strategies are always at the forefront of innovation and providing the tools necessary to lead a healthier, more predictable life with diabetes.
Resources:
Nutrition Foundation New Zealand
https://nutritionfoundation.org.nz/glycaemic-index-gi/
Diabetes UK